A NEW DISCIPLINE WAKES UP TO WOMEN’S SHUT-EYE PROBLEMS
STORY BY Elizabeth Heubeck PHOTOGRAPHY BY André Chung
Laura Jones (not her real last name) is, like a lot of moms, stretched thin. The 49-year-old Howard County resident juggles the needs of her three children and a home-based photography business with the recently added stresses of supporting friends going through challenging times — from difficult divorces to cancer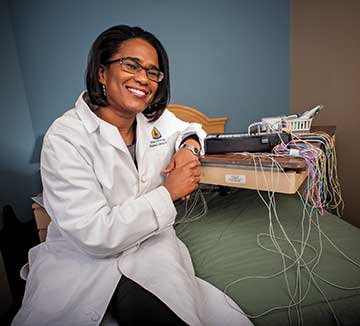 diagnoses. A few years ago, this hectic lifestyle began to catch up with her.
diagnoses. A few years ago, this hectic lifestyle began to catch up with her.
“I would push myself to stay up later and get only three to four hours of sleep. It worked for a while. Then I got to the point where I couldn’t sleep,” she says. For a period of approximately six months, Jones managed to get by on about 10 hours of sleep — a week.
Not surprisingly, the sleep deprivation took its toll. Jones recalls eating more than usual and consuming a lot more caffeine than she had in the past. These strategies, however involuntary, failed to compensate for her extreme sleep deprivation. “I got less and less productive during the day. When you aren’t sleeping, it’s hard to be efficient with anything,” Jones says.
Countless women can relate to Jones’ plight of sleeplessness. Approximately 63 percent of women experience symptoms of insomnia at least a few nights a week, according to the National Sleep Foundation (NSF). And although most adults require seven to nine hours of sleep nightly to function adequately the following day, a NSF poll found that women ages 30 to 60 average just six hours and 41 minutes of sleep per night, especially on weeknights. Beyond the next-day grogginess and irritability that often result from a sleepless night, long-term sleep deprivation can place women at risk for a laundry list of serious health ailments, including high blood pressure, stroke, cardiovascular disease, depression and diabetes.
Fortunately, the medical community is beginning to recognize the link between sleep patterns and overall health. The Johns Hopkins Center for Sleep at Howard County General Hospital is on the forefront of the emerging specialization of sleep medicine. Newly expanded in November of 2013, the center now offers an inpatient and outpatient clinic as well as the expertise of a multidisciplinary team of specialists from neurology, pulmonology and psychiatry/behavioral sciences.
“We are thrilled with the fact that sleep medicine is starting to resonate in the medical community and the general population,” says Charlene Gamaldo, M.D., medical director of the Johns Hopkins Center for Sleep. “It’s remarkable that in such a short span of time this subspecialty is getting so much attention.”
Even so, says Gamaldo, too many women, who are busy managing the lives and health of their family members, continue to dismiss their own sleep problems. In doing so, they place their long-term health at risk, Gamaldo adds. “Many women will say, ‘Oh well, that’s just how it goes’.” But sleep problems are nothing to take lightly. And, unfortunately, women are prone to them for a number of reasons.
WHY WE SOMETIMES FAIL AT SLEEP
Women, particularly those experiencing the hormone fluctuations associated with perimenopause and menopause, are at much greater risk for sleep problems.
While the medical community hasn’t embraced a direct correlation between declining levels of estrogen during perimenopause and subsequent sleep disturbances, the decrease in this hormone has been linked to hot flashes, which can in turn cause sleep disturbances. Moreover, during this ‘change of life’, a woman’s levels of progesterone — considered a sleep-promoting hormone — also decline.
In a “Huffington Post”article titled Menopause is the Ultimate Sleep Challenge, author OB/GYN Rebecca Booth, M.D. describes the effect of waning levels of hormones during menopause this way: “Yes, some menopausal women are experiencing a flight-or-fight reaction in the middle of the night due to the brain withdrawing from reproductive hormones that are no longer pouring out of the retiring ovary.”
Two other primary culprits of sleep disturbances, restless leg syndrome and sleep apnea, also increase among women undergoing menopause. In fact, a 2007 study published in the medical journal “Menopause” concluded that 53 percent of women over the age of 44 with sleep disturbances suffer either from restless leg syndrome or sleep apnea.
Sleep apnea is considered a serious sleep disorder. Its main physical symptom is snoring, which leads to interrupted breathing during sleep. Sleep studies of adults with sleep apnea have recorded as many as 100 breathing cessations during a single night’s sleep. Menopausal women are three to five more likely than the general population to develop sleep apnea, which is associated with increases in blood pressure, according to the NSF, as well as extreme daytime sleepiness due to all the nighttime sleep disturbances.
Restless leg syndrome, or RLS, provokes a strong urge to move one’s legs during sleep. Women are twice as likely to develop RLS as are men. Up to 25 percent of all pregnant women suffer from RLS, and those who do are more likely to experience it again later in life, according to Hopkins’ Gamaldo. Replacing iron stores is the first-line defense for RLS. However, explains Gamaldo, RLS can be a symptom of other medical problems, including diabetes and peripheral neuropathy.
GETTING BACK TO SLEEP
It’s not always easy to pinpoint the origin of sleep disturbances; finding a solution to the problem also may  take time.
take time.
“Sleep is one of those very complex and exquisite behaviors,” Gamaldo says. It’s not surprising, then, that treating patients with long-term chronic insomnia can take several months.
For many types of sleep disturbances, the Johns Hopkins Center for Sleep attempts behavioral interventions (see sidebar for sound sleep strategies) before considering sleep medications or hormonal replacements, explains Gamaldo.
Although it can take some time to identify the cause of sleep disturbances and return sufferers to restful nights of sleeping, the good news is this: once hormonal fluctuations associated with perimenopause and menopause subside, women’s sleep problems tend to resolve. Until then, they can be a silent, yet very real – even debilitating – health problem.
“The larger community is not going to get why you’re so disheveled. People don’t understand how brutal it is not to sleep,” says Jones, who reports being much better rested than she was a few years ago, thanks to a multidisciplinary approach to her insomnia. *
CREATING A SLUMBER-PRONE ZONE
– Allow yourself a two- to three-hour wind-down relaxation routine prior to bedtime
– Avoid going to bed full or hungry; both are mentally distracting.
– Exercise regularly, but not too close to bedtime as it can give you an adrenaline rush.
– If you suffer from hot flashes at night:
– Use a fan in your bedroom
– Minimize spicy foods close to bedtime
– Ensure pajamas and bed linens are made from breathable material, like 100% cotton
– Layer your night clothing so you can discard some of it during the night
– Avoid a large intake of liquid in the evening to minimize bathroom use in the middle of the night.
– If you suffer from repeated bouts of sleep disturbances, seek consultation from your doctor or a sleep center.
Source: Charlene Gamaldo, M.D., medical director of the Johns Hopkins Center for Sleep




